Breast Unit
Reconstruction using Implants
Reconstruction using an implant
 Mr Richard Sutton in Theatre |
On this page: Introduction The technique in more detail What are implants made of? Are Silicone implants safe Other Reconstructive Options General Hospital Information |
Introduction
Using an implant is the simplest technique to achieve a breast reconstruction. In essence it involves replacing the tissue that has been removed through surgery with a breast implant.
It is most often used to reconstruct the breast at the same time as the mastectomy but can also be used as a delayed technique. It is perhaps most useful after a bilateral mastectomy to reconstruct both breasts.
This approach can achieve good results, especially if aiming to reconstruct a relatively small breast and one that does not have much droop. Conversely it is not a good technique to make a larger breast or one that has a more mature shape with a significant droop.
Some of the benefits of this technique are that it does not involve the need to make scars elsewhere on the body and it is a relatively quick procedure that does not add much extra time to that of a mastectomy. The level of post-operative discomfort, the length of stay in hospital and the recovery period are reduced when compared to more complex methods that use a tissue flap.
However, there are some negative aspects that also need to be considered:
- This method creates a breast that is quite firm to touch and has little natural movement. So, it feels and moves very different to a real breast.
- It does not age like normal breast tissue either: it cannot loose or gain weight nor can it be affected by gravity. So, with the passage of time the level of symmetry between the reconstructed breast and the normal breast may deteriorate. In turn this may detract from the cosmetic result leading to the need for further surgery.
So, it is very important to understand that women who have a reconstruction that uses an implant will almost certainly require more surgery in the future.
Such procedures might include surgery to change the implant, to soften the scar tissue capsule that forms around the implant or surgery for to the other breast, to achieve a better match.
Technique in more detail
It is important to understand from the outset that this technique involves a number of different stages:
- Stage 1
involves placement of a temporary tissue expander implant; usually performed at the time of the mastectomy - Stage 2
involves having a number of injections of saline into the implant to allow for expansion of the skin and the muscle - Stage 3
involves a second operation to exchange the tissue expander for a permanent silicone implant
Stage 1
After the mastectomy has been completed a 'pocket' for the breast implant is made deep to the muscles of the chest wall; principally under the muscle fibres of pectoralis major.
It is important that the implant is protected under the fibres of this healthy muscle layer in order to reduce the risks of post-operative complications (such as infection) and it also helps to improve the shape and the contour of the reconstructed breast.
However, this muscle is naturally quite flat and needs to be stretched to become breast shaped. For this reason we normally insert a temporary tissue expander implant into the muscle pocket.
The tissue expander is partially inflated with salt water (saline). Afterwards the muscle is carefully closed over the expander implant and the skin will be sutured with a fine dissolvable stitch. A surgical drain is also placed in the wound to remove any tissue fluid or blood that will form underneath the skin of the reconstructed breast.
The scar that is left on the reconstructed breast is somewhat variable in length and position. However, in most cases it is a short transverse scar (5-6cm) on the front of the breast, where the nipple used to be.
The duration of the procedure is approximately three hours – when combined with a mastectomy and sentinel node biopsy.
The inpatient hospital stay is normally about 3 days following surgery. Obviously there is some discomfort in the chest area after surgery but it is normally fairly easy to control the discomfort with simple painkillers such as paracetamol aspirin.
Initially after the operation the reconstructed breast is swollen and bruised and may be quite distorted in shape and contour. It is important not to expect instant results. It takes many weeks and months before all of the post operative swelling subsides, before the tissues and skin can relax and stretch and before we can really judge what the final shape and size of the reconstructed breast is really like.
Sometimes it is necessary to undertake further surgical procedures to help improve the cosmetic result of the reconstruction or to treat complications that develop after surgery. However, it is always important to view breast reconstructive surgery as a process rather than as one single operation.
Most patients would not expect to develop problems and complications following this type of surgery but a percentage of patients may do so. This could include things like a wound infection delayed wound healing (or wound breakdown), as well as bleeding into the wound to form a collection of blood.
In general most of these types of problems can be effectively and quickly treated. However, if the wound does become infected there is a chance that this could compromise the breast implant. When this occurs it can sometimes be necessary to remove the breast implant for a period of time (many months) until the infection has been properly treated.
For those patients who are having a reconstruction at the time of their mastectomy it is important to understand that if problems and complications develop after surgery that occasionally it may be necessary to delay the administration of additional medical treatment such as chemotherapy or radiotherapy. Such a delay is uncommon and when it does occur it is likely to lead to a delay that is measured in days and weeks rather than in months.
Stage 2

Tissue Expander
Most women who have an implant based reconstruction (either as an immediate or certainly as a delayed procedure) will require tissue expansion, to stretch both the remaining skin of the chest wall and the muscle pocket that covers the implant.
This process of tissue expansion helps to form a breast mound with a more natural shape and can be a very useful technique even when the reconstruction is being undertaken at the same time as a mastectomy. Of course, good tissue expansion is absolutely essential if the operation is being performed in the delayed setting so that there is sufficient skin to cover the implant and also to create a more natural looking droop of the breast.
Skin is very elastic and has a surprising ability to stretch, as long as it has not been previously treated with radiotherapy. So, tissue expansion is not usually suitable for women who have had radiotherapy treatment as this will affect the elasticity and quality of the skin. It is also unsuitable for women with very large breasts as it is difficult to make a good match.
The expander implant is constructed of silicone and has a hollow chamber in the centre that can be filled with a variable quantity of saline (salt water solution).
The saline is injected via a port into the expander to increase its volume. There are two main types of port design:
- The port can be either be built directly into the front wall of the expander implant; or
- The port can be separate from the expander shell but is attached to the saline chamber with a plastic tube. In this instance the port is secured underneath the skin of the chest wall a few centimetres away from the expander itself (this maybe quite close to the implant or deep to the skin in the armpit).
The process of tissue expansion begins some weeks after the initial operation and when the wounds are looking healthy with good healing.
This is a gradual process that may take many weeks to complete, with injections being undertaken at intervals of one or two weeks apart. The amount of time taken to complete the expansion process will vary from person to person.
The injections themselves are usually undertaken in the outpatient clinic and this normally takes only a few minutes to perform.
When the breast expander implant is being filled you will feel a stretching sensation and tightness within the breast. It can be uncomfortable for a day or two after each inflation, but it should not be too painful.
The expander is generally inflated until the new breast is slightly larger than the other breast and then left for a few months to allow the skin to stretch. The excess fluid is then removed through the port so that the new breast droops slightly, with the aim of mirroring the other breast more closely.
Stage 3
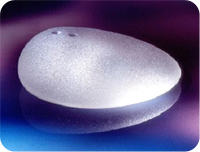
Teardrop shaped silicone gel implant
A further operation is normally needed to remove the expander and port and replace it with a permanent implant to create the final breast shape. This second operation is not thought of as major surgery and can often be performed as a day case basis, although it does require a short general anaesthetic.
This operation normally takes in the region of about 30 minutes. A new, small incision is made in the crease underneath the reconstructed breast. The tissue expander is removed.
The scar tissue capsule that has formed around the implant often needs to be adjusted slightly to help improve the shape of the reconstructed breast. A new implant is then inserted. This is the final permanent implant.
Usually this is a cohesive silicone gel implant, one with an anatomical (or teardrop) shape. The skin incision is then closed with a fine dissolvable suture, buried deep to the skin.
What are implants made of?
Breast implants have an outer shell made from silicone elastomer (similar to rubber). The shell is filled with silicone gel or saline. The surface of the implants may be smooth or textured, but at the Royal United hospital we would normally use textured implants.
Silicone gelMost permanent implants used for reconstruction surgery contain silicone gel and these tend to look more natural than saline implants. They are more robust, are less likely to leak and are less prone to develop ripples and creases on their surface. The silicone implants that we use at the RUH are made of something called cohesive silicone gel, with a consistency of 'Turkish delight'. The means that the silicone is not in liquid form; if the shell of the implant were to rupture the silicone contained within it cannot leak readily into the surrounding tissues. Silicone breast implants are manufactured in a whole range of styles, shapes and sizes. However, in general at the RUH we would normally prefer to use implants that have an anatomical (or teardrop) shape as we believe that these can give the best and most natural result. |
Teardrop shaped silicone gel implant |
Saline (salt water)Saline is an alternative to silicone gel, although the outer shell of the implant is still made of silicone. These implants contain a liquid rather than a gel and so are more likely to ripple under the skin and can sometimes leak. The solution is absorbed within the body and is not harmful, but as the saline leaks out the breast gradually gets smaller and the implant has to be replaced. Saline implants are also heavier, which may restrict the size that can be used. |
|
Expander implantsThis type of implant uses both silicone gel and saline. The outer shell is made of silicone and the inner shell is an expander implant with an adjustable saline filler. It is used in both immediate and delayed reconstructions. Once inserted, implants are very difficult to damage. This means that you can continue with all your normal activities including travelling by plane and taking part in sports. |
Tissue Expander |
Are silicone implants safe?
Silicone implants were first used in the early 1960s. During the 1980s many women, mainly in the US, began to link a range of illnesses with their silicone implants. They experienced various symptoms, from headaches to insomnia, extreme tiredness to loss of sex drive, and they felt that these were caused by leaks of silicone gel from their implants.
Experts have regularly examined all the evidence for and against silicone gel implants and have consistently concluded that they are not harmful.
Large clinical studies have been undertaken in the UK and in Europe to look at the safety of silicone implants and it has been shown that breast silicone implants are safe and that they do not pose any threat to long term health.
All implants sold in Europe have to pass strict safety checks and some of the manufacturers are starting to give a life long warrantee for some of their implants. So, surgeons are satisfied that they can be safely used in breast reconstruction and continue to recommend them to women considering surgery.
Modern silicone gel implants are expected to last 10 to 15 years, but there is no need to replace them after this time if there are no problems.
The Medicines and Healthcare Regulatory Agency (MHRA) has a publication called 'Information for women considering implants' which you may find useful. Visit www.mhra.gov.uk for more details.
Other Reconstruction Options
Reconstruction using flaps of muscle, fat and skin
Recovering after a breast reconstruction
Also see
Breast Cancer Care
Link opens in new window
Breast Cancer Care: Breast Reconstruction Link opens in new window
General Hospital Information
Your Hospital Stay (link opens a new window)
Transport & Parking (link opens a new window)


