Gastroenterology |
B57
|
Clinical Advice
Clinical Advice
We are happy to give clinical advice on weekdays via Cinapsis (a system that connects GPs to specialists) or for advice by email please contact us at ruh-tr.gastrosecs@nhs.net
Useful email contacts are also available here.
Cinapsis and the gastro secretaries inbox are checked on a daily basis during the working week by the departmental secretaries and enquiries distributed as appropriate. You may be able to find help with some queries in our FAQ section below.
The inbox is checked on a daily basis during the working week by the departmental secretaries and enquiries distributed as appropriate. You may be able to find help with some queries in our FAQ section below.
Frequently Asked Questions
Q: My patient has a low magnesium on PPI treatment, what can I do?
A: Options include lifestyle advice, alternative medication or magnesium supplements alongside PPI:
Lifestyle advice – dietary changes to increase magnesium consumption:
Magnesium is contained in a wide range of foods. In general, high-fibre foods (such as nuts, legumes, and leafy greens) contain magnesium, as well as various other sources such as some fortified cereals and electrolyte drinks. The recommended daily intake of magnesium is 300mg a day for men and 270mg a day for women aged 19 to 64 years. BBC Good Food have a range of high-magnesium recipes for people to try.
Alternatives to PPIs:
Depending on the indication of the PPI, there are alternative options:
- Dyspepsia – non-pharmacological measures (such as weight loss, stopping smoking, dietary changes), antacids (such as Gaviscon), or H2 antagonists may be appropriate
- Gastric ulceration – for maintenance of remission a H2 antagonist may be appropriate. PPIs should be used preferentially during active ulceration due to increased safety and efficacy (1)
- Gastroprotection – the ongoing need for the medicine with high risk of GI bleeds/ulceration should be reviewed and discontinued if possible
Long-term PPI use should be reviewed and stepped down as appropriate, as per BSW formulary guidelines.
Long-term magnesium supplements:
Magnesium glycerophosphate is licensed for prevention of recurrence of magnesium deficit at a dose of 24mmol (97.2mg). Patients should be encouraged to buy supplements over the counter; a dose of under 400mg a day is unlikely to cause harm. Acute hypomagnesaemia should still be treated as per local or national guidance.
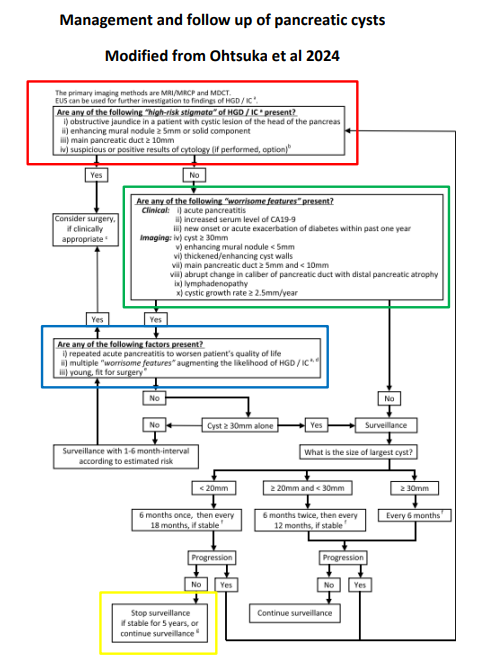
Q. My patient has been found to have a pancreatic cyst, they have asked if they will need a further scan, and where they might read more about it?
A. We have information available for patients here:
RUH Guidance for pancreatic cyst
Surveillance is delivered according to the guidance of the BRI Regional HPB team found here.
Q. My patient has been found to a gallbladder polyps – how do I determine the appropriate surveillance?
A. The RUH has published Gall Bladder Polyp Management Guidance; this approach is based on the current revised European guidance and can be reviewed here:
RUH Guidance for Gall Bladder Polyp Management
Q. Do patients with a positive TTG antibody need to have a small bowel biopsy to confirm the diagnosis of coeliac disease?
A. Yes. All patients should have histological confirmation of the diagnosis. It is best to refer initially for an endoscopy rather than to the outpatient clinic. The patient should be advised to be on a normal wheat containing diet for six weeks prior to the endoscopy. Shorter periods of including gluten in the diet are acceptable if this is all the patient can manage but may lead to less reliable results.
Q. How do I monitor my patient on IBD medications under shared care?
A. See below:
RUH Guidance for Monitoring of IBD Medications
Q. My patient with an enteral tube has a tube-related concern?
A. RUH enteral tube information:
Enteral Tube Problems - Information for patients, nursing and medical staff
Q. Should this patient with a family history of colon cancer have colonoscopy screening?
A. The British Society of Gastroenterology's current recommendations for screening individuals with a family history of colon cancer are available via this link:
Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups
High risk
People who have a three or more first-degree relatives under 50 years old (mother, father, brother, sister, child) who have had colorectal cancer or a Lynch syndrome cancer (endometrium, small bowel, ureter or renal pelvis) in > 2 generations; at least one affected relative must be no more than 50 years old at diagnosis and one of the affected relatives must be a first degree relative of the other two, or a known family history of a genetic syndrome, should be referred to the clinical genetics team to determine colonoscopy surveillance interval alongside referral for colonoscopy.
High-moderate risk
People who have a three or more first-degree relatives over 50 years old (mother, father, brother, sister, child) who have had colorectal cancer, or two affected relatives less than 60 years old in a first degree kinship with each other, or two affected relatives with a mean age less than 60 years old in a first-degree kinship should be offered five yearly colonoscopy from age 50 until 75 years and be referred to the clinical genetics team.
Moderate risk
People with only one first-degree relative affected by colorectal cancer aged under 50 years or with only two first degree relatives who have had colorectal cancer over 60 have a moderate risk of developing colorectal cancer. These people should be offered a single colonoscopy at age 55 years. If the investigation is normal, then no further investigations (other than the normal bowel cancer screening by FOB) are recommended.
Low risk
People with family histories that are different to those listed above are classified as low risk, as their risk is similar to the population in general. These people do not need any further investigations (other than the normal bowel cancer screening by FOB).
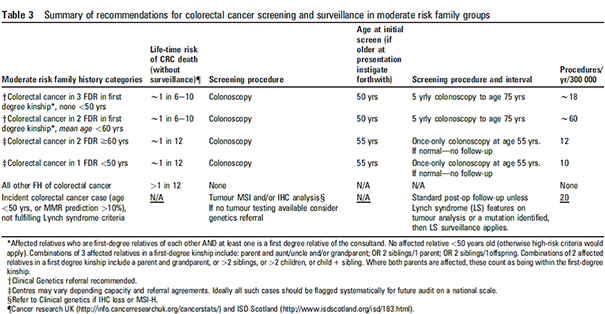
Click here to enlarge the summary above
Q. My patient has IBD, they have presented with a flare. Where can I seek advice?
A. We have information available for GPs managing IBD patients below:
Alternatively, you can contact the gastroenterology team via Cinapsis - e.g. if the pathway hasn't helped.
Patients can contact the IBD helpline on: 01225 825598 Monday to Friday between 8 - 11 Monday to Friday.
Q. I have a patient with IBD asking about Coronavirus?
A. See the documents below.
How can I find out about the affect of Coronavirus on my IBD?
We would recommend this resource:Coronavirus (COVID-19) advice for people with IBD