Acute Stroke Unit |
B6
|
Stroke Research


Stroke Research
Research is important because it helps to improve healthcare by finding out which treatments work best.
The stroke team is committed to providing the best possible care for our patients and our team includes research nurses who organise the studies and work with patients who take part in these studies.
We are part of the West of England Clinical Research Network and are involved in several national and international trials.
The studies are looking into various aspects of the care and treatment of patients who have had a stroke or TIA (mini stroke), including improving recovery and preventing further strokes, as well as looking for possible genetic causes of stroke.
All the research undertaken is approved by the trust, and is deemed to be ethical and safe. Participation is entirely voluntary, and does not affect normal patient care.
If you would like to know more about our studies and how you can participate, please contact the Stroke Research Team:
01225 824120
Further information about clinical trials
A 5-minute video from the Medical Research Council Clinical Research Unit.
Clinical Trials - What they are, and what they're not
A pamphlet from the National Institute for Health Research.
Understanding clinical trials
A pamphlet from the National Institute for Health Research.
How does clinical research takes place in the NHS?

OK to ask aims to encourage more patients or carers to ask about research opportunities.
Research Studies
Research Studies currently recruiting:
ENRICH AF: EdoxabaN foR IntraCranial Hemorrhage survivors with Atrial Fibrillation - The overall goal of this research is to establish the efficacy and safety of anticoagulation with edoxaban in individuals with AF and previous intracranial hemorrhage (intracerebral hemorrhage, intraventricular hemorrhage, subarachnoid hemorrhage and subdural hematoma).
Evolocumab: A Double-blind, Randomized, Placebo-controlled, Multicenter Study to Evaluate the Impact of Evolocumab on Major Cardiovascular Events in Patients at High Cardiovascular Risk Without Prior Myocardial Infarction or Stroke.
OPTIMAS: Optimal TIMing of Anticoagulation after acute ischaemic Stroke - a randomised controlled trial to compare whether starting a DOAC within 4 days of cardioembolic ischaemic stroke is more beneficial compared to the existing usual treatment (starting a DOAC at 7 to 14 days after a stroke).
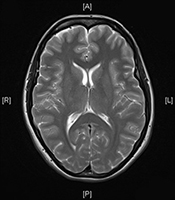
PLORAS: Predicting Language outcome and recovery after stroke - The aim of the study is to provide a clinical protocol that will Predict Language Outcome and Recovery After Stroke (PLORAS). The system we are developing takes a structural brain image of a new participant with language difficulties (aphasia) and produces probabilistic estimates of long term outcome, based on whether, when, and in what respects, other participants with "matching" lesions recovered their speech and language abilities – read more
SETICOS: Study Exploring The Impact of COVID 19 on stroke - This study is looking to assess how infection with COVID-19 affects stroke mortality, stroke recurrence and early outcome at the end of their acute admission by comparing these features in acute stroke patients with and without evidence of concurrent COVID-19 infection at the time of their stroke.
PhEAST: Pharyngeal Electrical stimulation for Acute Stroke dysphagia Trial - This study is assessing whether Pharyngeal Electrical Stimulation is safe and effective at improving post-stroke dysphagia.
TICH-3: Tranexamic acid for hyperacute spontaneous IntraCerebral Haemorrhage - This study is assessing the clinical effectiveness of TXA after ICH and determine whether Tranexamic acid should be used in clinical practice.
Recently published trials in which RUH patients participated:
INTERACT2: Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial. The INTERACT2 study found that patients who suffered an acute intracerebral haemorrhage and received fast blood pressure lowering treatment within 6 hrs were better off both physically and psychologically. This treatment regime has since been implemented here at the RUH.
SO2S: Stroke Oxygen Study: A multi-centre, prospective, randomised, open, blinded-endpoint study to assess whether routine oxygen treatment in the first 72 hours after a stroke improves long-term outcome: There is no evidence to support giving routine Oxygen to stroke patients. The study found that there was no difference in outcome between the 3 trial groups (O2 given at night for 3 nights, continuous O2 for 72 hours or no oxygen). Therefore we need to continue our normal practice of monitoring patients routinely and only give Oxygen if indicated according to patients' SaO2.
ENOS: The 'Efficacy of Nitric Oxide in Stroke' (ENOS) study is a controlled trial designed to test the safety and efficacy of transdermal glyceryl trinitrate (a nitric oxide donor) or control; and continuing or temporarily stopping prior anti-hypertensive medication. No difference in outcome was found in the GTN groups. Also, there was no evidence to support continuing pre-stroke blood pressure medication in patients in the acute phase of stroke. Of particular interest was that patients who did continue oral BP medication - despite having swallowing problems - had a higher incidence of pneumonia. Therefore, antihypertensive medication can be continued once the patient is stable and safe enteral access has been established.
IRIS - The Insulin Resistance Intervention after stroke trial - a randomised placebo-controlled trial of pioglitazone, compared with placebo, for prevention of stroke and myocardial infarction after ischemic stroke and transient ischemic attack.
In this multi-centre, double-blind trial, Patients were randomly assigned either pioglitazone or placebo. This trial involved patients without diabetes who had insulin resistance along with a recent history of ischemic stroke or TIA, the risk of stroke or myocardial infarction was lower among patients who received pioglitazone than among those who received placebo. Pioglitazone was also associated with a lower risk of diabetes but with higher risks of weight gain, edema, and fracture. (Funded by the National Institute of Neurological Disorders and Stroke)
This was a landmark study demonstrating that treatment of insulin resistance in stroke survivors reduces the subsequent risk of stroke and myocardial infarction.

